-

For the man
who wants to finish his workday -

For the man
who wants to enjoy the movie -

For the man
who wants to sleep
through the night
In clinical studies, most men who received Aquablation therapy preserved continence, erections, and ejaculation.1
The Outcomes Men Deserve
Significant symptom improvement2
of patients avoided another BPH intervention at 5 years1,2
EMBRACE LIFE AGAIN WITH AQUABLATION THERAPY
For men with BPH seeking a normal, uncompromised life, Aquablation therapy offers a minimally invasive, effective solution for lower urinary tract symptoms (LUTS) caused by BPH. Using robotic precision, Aquablation therapy delivers lasting results with a low risk of complications, empowering you to live confidently on your terms.
A ONE-OF-A-KIND PROCEDURE
Aquablation therapy is the only real-time, ultrasound-guided, robotic-assisted, heat-free waterjet for the treatment of BPH.
Step 1. Surgical Planning
Watch how surgeons create a personalized treatment plan that determines which tissue to resect and preserve before an Aquablation therapy procedure.
Step 2: Prostate Tissue Removal
See how Aquablation therapy precisely resects prostate tissue while preserving surrounding areas with the guidance of a treatment plan.
See Howard's BPH journey
Success stories
See how men regained their quality of life by choosing Aquablation therapy for BPH relief.
1 in 2 Men Between 51-60 Report They Have BPH3
Living with BPH has many challenges. Understanding the condition and its effects is key in the journey to find relief.
The BPH Symptom Assessment
Answering these questions can help you and your urologist measure the severity of your BPH symptoms.
Understanding your options
Aquablation therapy is a safe and effective treatment for patients suffering from LUTS due to BPH. It can be performed on prostates of any size and shape.1,2
Aquablation therapy is a one-of-a-kind procedure. It is the only procedure that uses a heat-free waterjet controlled by robotic-assisted technology to resect prostate tissue.
ADDITIONAL TREATMENTS
If a patient determines that his BPH symptoms are not bad enough to start treatment, he can choose watchful waiting.4
This means that before considering any medical treatment, the doctor and patient wait to see if symptoms get worse or new symptoms develop.
Medications are often the first step in treating BPH. They are prescribed by your doctor to address your symptoms by either shrinking (5-alpha reductase inhibitors) or relaxing (alpha-blockers) the prostate.5 In some instances, patients may be prescribed a combination of both medications.
Surgery—including Aquablation therapy—may be a longer-lasting treatment for BPH. There are two types of surgical treatments: resective and non-resective.
In resective procedures, some or most of the prostate tissue is removed during the procedure, so they are generally longer-lasting than non-resective procedures.6 In non-resective procedures, prostate tissue is not removed at the time of surgery.
How does Aquablation therapy work?

Step 1. Surgical Planning
With the help of ultrasound imaging, doctors can create a detailed guide to plan the procedure. This guide outlines the specific areas of the prostate that need removal. The tissue within the marked area of the prostate may be removed, while the tissue outside of it may remain untouched.

Step 2. Removing the Prostate Tissue
Next, a robotic-assisted system follows the surgical plan and resects the targeted prostate tissue using a heat-free waterjet. This advanced technology helps ensure precise, consistent, and predictable removal of the tissue.
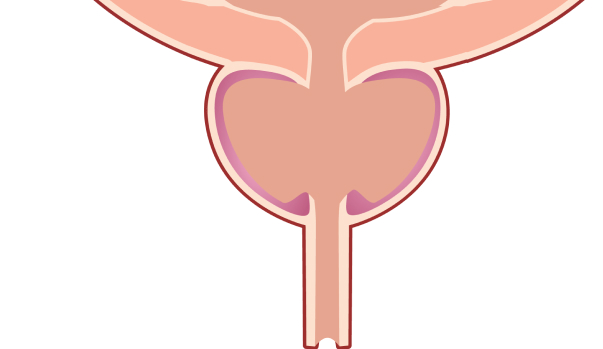
Step 3. Prostate After Treatment
After the procedure, urine flows normally from the bladder, passing through the treated prostate, and exits the body.
This depiction is for illustrative purposes only and does not indicate clinical performance. Patient responses can and do vary.
References:
- Elterman D, et al. BMJ Surg Interv Health Technol. 2021.
- Gilling PJ, et al. Can J Urol. 2022.
- Roehrborm CG, et al. Clin Interv Aging. 2008.
- Mayo Clinic. Benign Prostatic Hyperplasia (BPH). 2024.
- Yale Medicine. Enlarged Prostate (Benign Prostatic Hyperplasia). 2024.
- Urology Care Foundation. 2019.